Top Qs
Timeline
Chat
Perspective
Desloratadine
Allergy medication From Wikipedia, the free encyclopedia
Remove ads
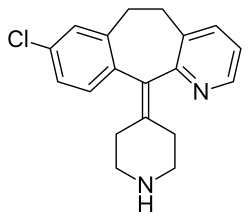
Desloratadine, sold under the brand name Aerius among others, is a tricyclic H1 inverse agonist that is used to treat allergies. It is the major active metabolite of loratadine.
It was patented in 1984 and came into medical use in 2001.[8] It was brought to the market in the US by Schering Corporation, later named Schering-Plough.[3]
Remove ads
Medical uses
Desloratadine is used to treat allergic rhinitis, nasal congestion and chronic idiopathic urticaria (hives).[9] It is the major metabolite of loratadine and the two drugs are similar in safety and effectiveness.[9] Desloratadine is available in many dosage forms and under many brand names worldwide.[10]
An emerging indication for desloratadine is in the treatment of acne, as an inexpensive adjuvant to isotretinoin and possibly as maintenance therapy or monotherapy.[11][12][13]
Remove ads
Side effects
The most common side effects are fatigue (1.2%), dry mouth (3%), and headache (0.6%).[14][9]
Interactions
Co-administration with erythromycin, ketoconazole, azithromycin, fluoxetine, or cimetidine resulted in elevated blood plasma concentrations of desloratadine and its metabolite 3-hydroxydesloratadine in studies. However, no clinically relevant changes were observed.[3][15]
Pharmacology
Summarize
Perspective
Pharmacodynamics
Desloratadine is a selective H1-antihistamine which functions as an inverse agonist at the histamine H1 receptor.[16]
At very high doses, is also an antagonist at various subtypes of the muscarinic acetylcholine receptors. This effect is not relevant for the drug's action at therapeutic doses.[17]
Pharmacokinetics
Desloratadine is well absorbed from the gut and reaches highest blood plasma concentrations after about three hours. In the bloodstream, 83 to 87% of the substance are bound to plasma proteins.[15]
Desloratadine is metabolized to 3-hydroxydesloratadine in a three-step sequence in normal metabolizers. First, N-glucuronidation of desloratadine by UGT2B10; then, 3-hydroxylation of desloratadine N-glucuronide by CYP2C8; and finally, a non-enzymatic deconjugation of 3-hydroxydesloratadine N-glucuronide.[18][19] Both desloratadine and 3-hydroxydesloratadine are eliminated via urine and feces with a half-life of 27 hours in normal metabolizers.[15][20]

It exhibits only peripheral activity since it does not readily cross the blood–brain barrier; hence, it does not normally cause drowsiness because it does not readily enter the central nervous system.[21]
Desloratadine does not have a strong effect on a number of tested enzymes in the cytochrome P450 system. It was found to weakly inhibit CYP2B6, CYP2D6, and CYP3A4/CYP3A5, and not to inhibit CYP1A2, CYP2C8, CYP2C9, or CYP2C19. Desloratadine was found to be a potent and relatively selective inhibitor of UGT2B10, a weak to moderate inhibitor of UGT2B17, UGT1A10, and UGT2B4, and not to inhibit UGT1A1, UGT1A3, UGT1A4, UGT1A6, UGT1A9, UGT2B7, UGT2B15, UGT1A7, and UGT1A8.[19]
Pharmacogenomics
2% of Caucasians and 18% of people from African descent are desloratadine poor metabolizers. In these people, the drug reaches threefold higher plasma concentrations at seven hours after intake, and it has a half-life of 89 hours (compared to a 27-hour half-life in normal metabolizers). Adverse effects were reported at similar rates in poor metabolizers, suggesting that it is not clinically relevant.[15][20]
Remove ads
References
Further reading
Wikiwand - on
Seamless Wikipedia browsing. On steroids.
Remove ads